Among the most prevalent causes of dizziness and imbalance in the senior population are benign paroxysmal positional vertigo in addition to different kinds of vertigo, which impair standard of life and raise the risk of falls, accidents, and loss of independence. The primary cause of BPPV is the displacement of tiny calcium crystals (otoconia) within the otolith organs into the inner ear’s semicircular canals, which results in transient bouts of vertigo brought on by head movements.
Table of Contents
ToggleA significant percentage of dizziness complaints in older persons are caused by vestibular dysfunction, including BPPV, which frequently coexists with other neurological and sensory problems that worsen balance. Because of these intricate interactions, we will be discussing the 7 reasons of bppv in geriatrics & its rehab to understand vertigo in older persons as it is a multifaceted issue that needs focused evaluation and treatment.
7 Reasons of BPPV in Geriatrics & its Rehab
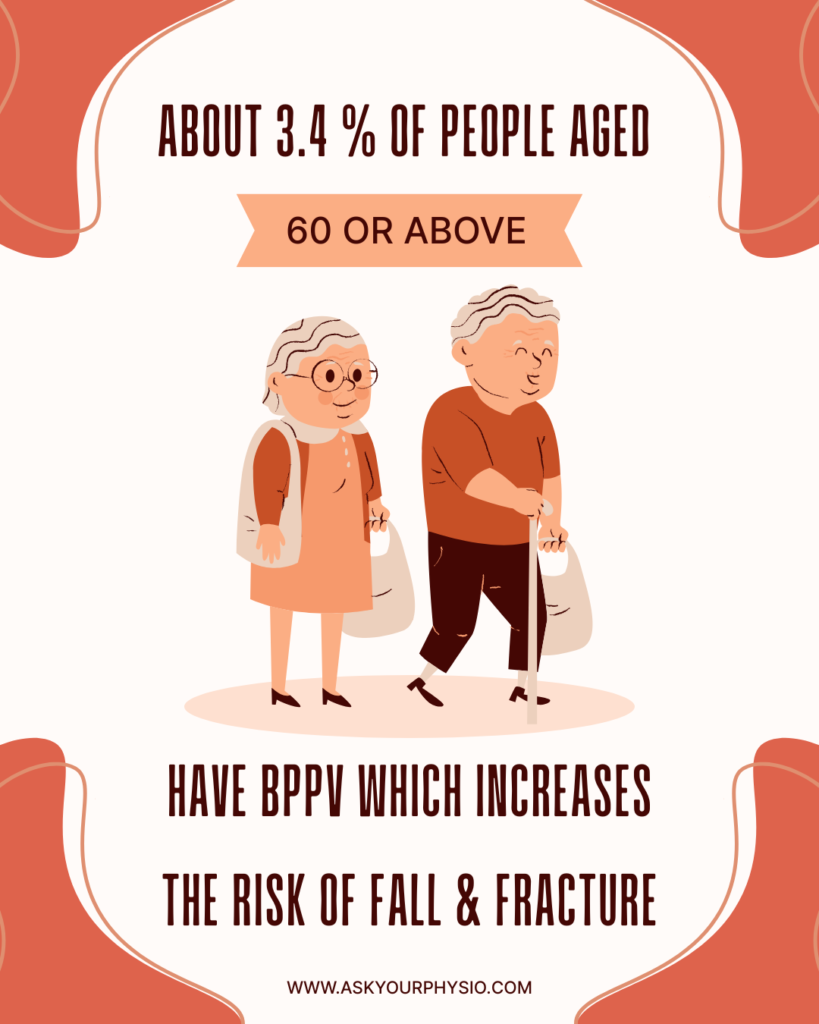
Benign Paroxysmal Positional Vertigo is the most prevalent root of vertigo presentations in healthcare settings, accounting for 20 to 30% of vestibular vertigo diagnoses in skilled dizziness clinics. According to one poll, 86% of people with BPPV said that their symptoms interfered with their normal daily lives, necessitating medical attention or reducing their ability to function. Lets dive into the 7 reasons of BPPV in geriatrics & its rehab.
Otolith Degeneration & BPPV
Among the 7 reasons of bppv in geriatrics & its rehab, the first one is age related otolith degeneration. In geriatrics, biological degeneration & transience of otoconia in the inner ear inclines them to BPPV because there is a greater chance that these crystals might tumble into semicircular canals, resulting in episodic vertigo. In these situations, positional vertigo brought on by motions like lying down or looking up is common, and the Epley canalith repositioning technique has been shown time and time again to dramatically reduce symptoms and enhance quality of life. Epley and related canalith repositioning techniques dramatically lessen vertigo and related discomfort in BPPV patients.
Symptoms
- Short bouts of positional vertigo, particularly when looking up, getting out of bed, or turning in bed.
- Feeling unsteady or instability when walking or standing
- A feeling of shifting or movement as opposed to constant spinning
- Nausea
- A greater fear of falling, which results in decreased activity
Rehabilitation
To swiftly and safely relocate displaced otoconia and alleviate vertigo symptoms, a qualified physical therapist or vestibular specialist should perform the Epley maneuver and other repositioning procedures.
Sarcopenia
A higher incidence of BPPV in older persons is linked to sarcopenia (loss of muscle mass) and concomitant body composition abnormalities, such as obesity and dynapenia, according to recent studies. In addition to causing imbalance, weak muscles and a slow gait make it more difficult to correct for vestibular dysfunction.
Symptoms
- Noticeable unsteadiness when walking and standing, particularly following episodes of positional vertigo
- Reduced step length and slower gait speed
- Increased exhaustion while performing daily tasks
- Inadequate recovery of balance following head movements or rotations
Rehabilitation
For older persons with sarcopenia, a focused physical therapy program that incorporates strengthening exercises, balance training, and practical movement training can assist enhance postural control and gait stability. Fall risk can also be decreased through pairing dynamic balance exercises with resistance training, such as lower body strengthening.
Vestibular Hypofunction
The third cause of bppv in geriatrics among the 7 reasons & its rehab is the vestibular hypofunction. In the elderly, vestibular hypofunction, a condition in which the balance system fails to react appropriately to head or body motion, often coexists with BPPV and exacerbates dizziness and unsteady walking. Nearly one-third of older persons with BPPV also have vestibular hypofunction, which worsens postural control, according to research. There are several causes of vestibular hypofunction, including trauma, significant injury to the vestibular end-organ, or an underlying vestibular condition such as vestibular neuritis.
Symptoms
- Oscillopsia, or blurry or bouncing vision, accompanied by head twists or walking
- Increasing instability in dimly lit or congested areas
- Having trouble staying balanced, especially on uneven ground
Rehabilitation
The main goals of vestibular rehabilitation treatment (VRT) are to enhance sensory integration, adaptation to motion sources, and vestibulo-ocular reflex function. The central nervous system can compensate for vestibular deficiencies with the aid of particular head motion exercises, gaze stability, and balance retraining. When discussing the 7 reasons of bppv in geriatrics & its rehab, the vestibular rehabilitation treatment can be availed for multiple etiologies.
Cardiovascular concerns & Blood Pressure
Older adults frequently suffer from cardiovascular conditions and blood pressure fluctuations, including orthostatic hypotension, which can cause lightheadedness or instability. Balance impairment can potentially be exacerbated by age-related vascular changes that impact blood flow to the inner ear and primary balance centers. Although the exact cause of age associated with cellular death in the vestibular endorgan is unknown, it is believed that oxidative stress and genetic predisposition may both be significant factors.
Symptoms
- Short term blurring or darkening of vision, particularly after abrupt postural adjustments
- Swaying or being unsteady when standing or moving
- feeling dizzy or on the verge of syncope, especially after extended sitting or reclining
Rehabilitation
To enhance cardiovascular conditioning and lessen dizziness associated with blood pressure swings, physical therapists can use graded aerobic exercise, controlled mobility exercises, and orthostatic tolerance training. In these situations, coordination with professional management is essential.
Sensory Deficits
The vestibular, ocular, and proprioceptive senses are all necessary for balance. Due to age, older persons frequently have reduced proprioceptive feedback or visual impairment, which can compromise postural control and make them more prone to imbalance and vertigo.
Symptoms
- A greater dependence on visual signals to maintain stability
- increased fear of falling and decreased mobility in general
- Perception of balance is impacted by blurry or double vision
Rehabilitation
To enhance postural control, physical therapy uses proprioceptive tasks, eye-head coordination exercises, and sensory integration training.
Neurological Disorders
Dizziness and vertigo are common symptoms of neurological problems in older adults, such as cerebrovascular events, central balance dysfunction, or age-related alterations in neuronal integration. Peripheral vestibular deficits may be mimicked or made worse by these illnesses. The simultaneous processing of somatosensory, visual, and vestibular cues to the neurological system, subsequently followed by outputs to the musculoskeletal system, maintains postural stability.
Symptoms
- Occasional weakness, tingling, or numbness in the limbs
- Diminished fine motor control when transferring or walking
- Clumsy gait
- Delayed response to changes in posture
Rehabilitation
Therapists can increase functional mobility and minimize dizziness related limitations among individuals with neurological disorders by using task-specific balance conditioning, gait modification, dual-task exercises, and cueing techniques.
Vitamin B12 Deficiency
The reversible role of vitamin B12 insufficiency in neuropathy, dizziness, and balance issues in older persons is becoming more widely acknowledged. Low B12 levels can cause or exacerbate unsteadiness by affecting proprioception, sensorimotor integration, and nerve function. Clinical case studies have shown that considerable B12 insufficiency was seen in older persons with unidentified gait disturbance and dizziness, and that symptoms resolved with proper treatment.
Symptoms
- Lightheadedness and dizziness, frequently brought on by movement
- Tingling, numbness, or “pins and needles” in the hands or feet
- Weariness or widespread weakness
Rehabilitation
To restore lost proprioceptive function and enhance dynamic stability, physical therapy should incorporate gait retraining, balance exercises, and sensory-motor coordination practice in addition to medical correction of B12 insufficiency (supplementation or injections overseen by a doctor). When compared to dietary correction alone, combination therapy frequently produces better functional results.
Points to Ponder!
BPPV and vertigo in older persons are frequently multifactorial, resulting from chronological otolith degradation, sarcopenia, vestibular hypofunction, cardiovascular problems, sensory impairments, neurological disorders, and dietary deficiencies such as vitamin B12 deficiency. All of these variables not only cause dizziness and imbalance, but they also dramatically raise the risk of falls, accidents, and a lower quality of life. Recognizing the underlying reason is critical to good treatment.
Vestibular rehabilitation, canalith repositioning procedures, balance training, strength exercises, and sensory integration treatment have all been shown to effectively alleviate symptoms and restore functional stability. Early intervention, which combines medical treatment and physiotherapy, can help older persons restore confidence, increase mobility, and minimize the risk of falling, thereby increasing their sense of autonomy and quality of life.
Read our previous blog AI Devices in Cardiac Rehabilitation
This article has been written by a Physical Therapist and provides general guidance on physical health & exercise. While it is grounded in professional expertise, it is not a substitute for individualized medical advice. If you are experiencing pain, specific symptoms, or have an underlying medical condition, please book a 1 on 1, 30 minute consultation with our expert physical therapist for a personalized assessment & tailored recommendations.
