Understanding the Anatomy
Although many individuals believe that a slipped disc is the root cause of their sciatica and lower back pain, this isn’t necessarily what happens. When it comes to sciatica diagnosis, disc vs piriformis remains one of the biggest challenges for both patients & clinicians. The spine can be thought of as a modified elastic rod due to the elasticity of the ligaments flavum, the longitudinal ligaments’ ability to absorb shock, and the flexibility of the spinal column. Body posture has an impact on how much strain is placed on the spine.
Table of Contents
ToggleWhat is a Herniated Disc?
Although the discs are quite adept at withstanding compression forces, they are most susceptible to abrupt shocks, especially when the vertebral column is bent and the disc is experiencing degenerative alterations that encourage nucleus pulposus herniation. The discs inclined to herniate are found in the lumbosacral region, which is where a mobile segment of the column joins a more immobile component. In such spaces, the posterior aspect of the annulus fibrosus ruptures & the nucleus pulposus is compelled posteriorly.
A disc injury typically results in an episode of back pain that travels throughout the leg and foot due to the pinched nerve’s distribution. With the most frequent compression of the posterior sensory roots of L5 and S1, pain typically radiates to the foot from the back and lateral side of the leg. This is known as sciatica. In extreme situations, there may be sensory loss or even paraesthesia involved. Accurate sciatica diagnosis: disc vs piriformis is crucial because the treatment path can differ completely.
Most Common Sites of Disc Herniation
A key part of sciatica diagnosis: disc vs piriformis, lies in understanding where the pain originates. While doing so, we need to understand the common sites of herniation. Most frequently, the discs between the L4 and L5 vertebrae or the L5 vertebra and the sacrum are impacted. Usually, the nerve roots that go to the intervertebral foramen below are affected by a posterolateral herniation, which misses the neighbouring nerve roots.
Causes of Disc Herniation
- Aging
- Trauma
- Recurrent strain
- Genetic predisposition
- Poor posture
Why is Piriformis Syndrome crucial?
Originating from the anterior surface of the sacrum, the faceted piriformis muscle is found in the buttock area exiting the greater sciatic foramen. It is responsible for the external rotation of the hip. When the piriformis muscle strains the sciatic nerve with pressure, it results in piriformis syndrome. This could occur as a result of prolonged sitting, direct trauma to the buttock area, improper weight lifting or even due to any scar tissue.
Because the clinical presentations of disc herniation and piriformis syndrome are frequently similar, clinicians often face the tricky task of sciatica diagnosis: disc vs piriformis. However, a competent therapist can distinguish between the two ailments due to slight differences.
Diagnostic Tests for Sciatica: Disc vs Piriformis
Imaging and diagnostic testing are essential for determining the cause of any persistent back or leg pain that a patient may be experiencing. Distinguishing between muscular reasons such as piriformis syndrome and spinal disc disease might be difficult which is why Sciatica diagnosis: Disc vs Piriformis requires careful tests for clinical interpretation.
Since an MRI (Magnetic Resonance Imaging) produces incredibly detailed images of the soft tissues, nerves, and spinal discs, it is typically the first option. While piriformis syndrome may not directly cause changes in the spine, it may cause inflammation around the muscle area. On MRI, a herniated disc pressing on the sciatic nerve root will usually be seen.
A computed tomography (CT) scan provides a closer look at the spine’s bony structures. When MRI is unavailable or when doctors wish to evaluate spinal canal constriction or degenerative changes that could resemble sciatica symptoms, it is especially helpful.
X-rays can show bone spurs, spinal deviations or fractures that may cause nerve discomfort, but they are less precise for changes in soft tissues. They aid in ruling out other underlying reasons, even if they cannot immediately demonstrate a herniated disc or muscular compression.
A PET scan (Positron Emission Tomography) may be used to diagnose uncommon or complicated situations. By highlighting regions of aberrant metabolic activity, this imaging might help identify inflammation or differentiate nerve-associated pain from other illnesses including tumours or systemic disease.
Ultimately, all answers cannot be found through a single diagnostic test. Findings must be interpreted by the doctor or physical therapist in light of the patient’s medical history and physical examination. This careful process ensures that Sciatica diagnosis: Disc vs Piriformis is accurate, guiding the treatment plan towards targeted and effective relief.
Clinical Case Study
Let’s evaluate a case study explaining this difference even further:
A 66 year old male patient presented to my clinic with MRI findings showing both anterior and posterior disc herniations. In October 2023, he claimed to have fallen in the shower and blamed a suspected disc slip for the pain that was radiating down his leg. He reported having trouble bearing weight on his foot when walking, as well as numbness and intense pain.
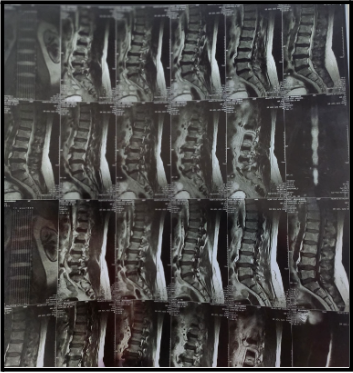
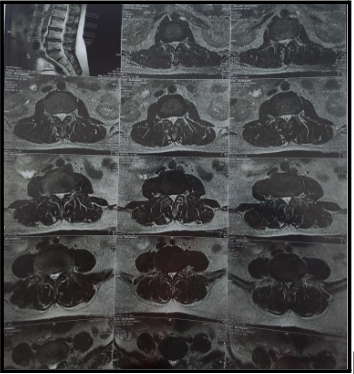
This MRI reveals:
- No evidence of fracture, listhesis or generalized marrow abnormalities.
- However, diffuse posterior annular bulge of L3-4 intervertebral disc is causing compression of the thecal sac and indentation of lateral recesses.
- Circumferential bulge of L4-5 intervertebral disc causes compression of thecal sac, bilateral lateral recesses and indentation of transiting nerve roots along with moderate narrowing of the spinal canal.
- Right posterior para central bulge of L5-S1 intervertebral disc causes effacement of epidural fat
- Compression of right lateral recess & right transiting S1 nerve roots
- Moderate narrowing of CSF column is seen on MR myelogram
- Anterior & posterior osteophyte formation is seen at L3, L4 & L5
The importance of detailed examination
However, a clinical examination showed that the piriformis was the persistent location of his pain. According to a comprehensive clinical examination, the patient’s pain increased with hip internal rotation instead of lumbar flexion, which is in line with piriformis syndrome. The Slump test initially came back negative, but the Straight Leg Raise (SLR) test produced buttock pain. The diagnosis of piriformis syndrome was further confirmed by a positive FAIR test.
Additionally, he reported that his pain was primarily limited to his buttocks, developed gradually, and tended to get worse when he climbed stairs. Furthermore, his symptoms did not get worse when he coughed or sneezed, two behaviours that are frequently linked to disc related discomfort. This finding led to a more thorough analysis that went beyond the imaging findings. Such findings hold a very special value when ruling out sciatica diagnosis: disc vs piriformis.
By successfully ruling out disc herniation as the main reason, these results saved the patient from having a discectomy as a first line of treatment. This highlights how sciatica diagnosis: disc vs piriformis depends heavily on thorough clinical examination, making it a vital part of history taking.
It enables the therapist to precisely determine the root cause of a patient’s symptoms, particularly in situations when imaging alone might not give the whole picture. In this instance, the patient’s symptoms and physical reactions did not correspond with typical disc-related sciatica, despite the MRI showing disc herniations. The therapist was able to identify that the discomfort was caused by piriformis syndrome rather than the spine by conducting a thorough evaluation that included hip movement testing, piriformis palpation, and specific inducement tests like the FAIR and Straight leg raise test
Once the source of pain is identified, the next step is management. You can read more in our detailed discussion on Can AI really treat your Sciatica? Myth or Truth?
What patients should know in Sciatica Diagnosis: Disc vs Piriformis
For patients one of the most important aspects of sciatica diagnosis: disc vs piriformis is learning to recognize their own symptoms. While sciatica associated with the piriformis typically feels tighter and intensifies after prolonged sitting or ascending stairs, a herniated disc frequently causes intense, shooting pain that gets worse when you sit, bend, or cough. Patients can have more effective conversations with their healthcare practitioner and begin the appropriate treatment sooner if they are aware of these distinctions.
Additionally, patients should be aware of when to see their physiotherapist. In physiotherapy practice, sciatica diagnosis: disc vs piriformis is considered one of the most discussed differential diagnoses. Considering that, if the symptoms increase with activity, last longer than a few weeks, or start to produce weakness or numbness, a professional evaluation is necessary.
This article has been written by a Physical Therapist and provides general guidance on physical health & exercise. While it is grounded in professional expertise, it is not a substitute for individualized medical advice. If you are experiencing pain, specific symptoms, or have an underlying medical condition, please book a 1 on 1, 30 minute consultation with our expert physical therapist for a personalized assessment & tailored recommendations.

Pingback: Expert Stress Relief Methods with Physiotherapy
Pingback: 6 Best Exercises to Treat Piriformis Sciatica -
Pingback: 10 Hidden Insights about Pelvic Floor Rehab -
Pingback: An Unparalleled insight into Plantar Fasciitis -